Maternal Mortality Rates in Africa: A Silent Emergency
- hearthiveorg

- Jul 18, 2025
- 5 min read
Updated: Aug 21, 2025
Across many African countries, maternal mortality rates remain alarmingly high despite global efforts to improve maternal health. Women in sub-Saharan Africa are disproportionately affected, with thousands dying each year due to preventable or treatable complications related to pregnancy and childbirth.
The leading causes of maternal mortality rates in African countries are often linked to deeply rooted issues—ranging from poverty and limited access to healthcare, to sociocultural barriers and systemic gender inequality.
Hemorrhage, hypertensive disorders such as eclampsia, unsafe abortions, and infections are among the most common direct causes. These are compounded by indirect factors like malnutrition, HIV/AIDS, and the absence of skilled birth attendants.

In rural or under-resourced areas, many women give birth without any medical supervision, increasing the risk of fatal complications. Additionally, poor infrastructure, lack of transportation, and the scarcity of equipped health facilities contribute to delays in receiving timely care, further exacerbating maternal mortality rates.
This crisis is not just a health issue—it is a human rights concern that reflects broader inequalities in access to education, economic opportunities, and decision-making power for women. While progress has been made through community health programs, charity efforts, and international aid, the rate of improvement remains slow.
Addressing the leading causes of maternal deaths in Africa requires a multi-sectoral approach that includes education, healthcare reform, and community empowerment. Without urgent, targeted intervention, thousands of women will continue to lose their lives during what should be a time of joy and new beginnings.
Leading Causes of High Maternal Mortality Rates in African Countries
Malnutrition on Maternal and Neonatal Health

Malnutrition significantly heightens the risk of maternal mortality rates in Africa. Poor nutrition weakens a mother’s immune system, making her more susceptible to infections, anemia, and delivery complications. Nutrient deficiencies such as iron, folate, and calcium directly affect pregnancy outcomes, increasing the risk of stillbirths, premature labor, and low birth weight.
Malnourished mothers often give birth to undernourished infants who face a higher chance of early death. In regions with food insecurity, expectant mothers may lack access to basic prenatal vitamins or balanced diets, further endangering their health and the survival of their newborns.
Hemorrhage, Infections, Unsafe Abortions, Hypertensive Disorders
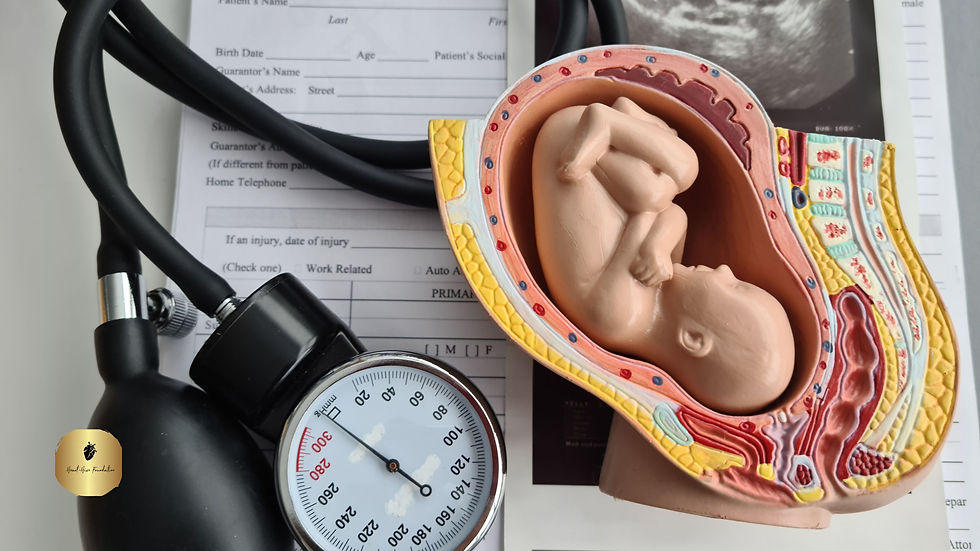
The leading medical causes of maternal mortality rates in Africa are postpartum hemorrhage, sepsis (infections), unsafe abortions, and hypertensive disorders like eclampsia. Hemorrhage—often due to delayed or poor-quality care—is the single most common cause of maternal death. Infections stemming from unhygienic delivery conditions or untreated postpartum complications are also widespread.
Unsafe abortions, typically carried out without medical supervision, often lead to fatal bleeding or infection. Hypertensive disorders, such as preeclampsia, are life-threatening when left untreated, especially in areas lacking diagnostic tools and trained staff. These causes are mostly preventable with timely, skilled obstetric care and proper prenatal monitoring—making this not only a medical issue but a social justice imperative.
Teenage Pregnancy
Teenage pregnancy is a major contributor to high maternal mortality rates in Africa. Young girls’ bodies are often not fully developed for childbirth, making them more prone to complications such as obstructed labor, fistula, and hemorrhage. Adolescents are also less likely to receive prenatal care or deliver in health facilities, increasing risks for both mother and baby.
Social stigma, early marriages, lack of education, and limited reproductive health access compound the issue. Teenage mothers face higher risks of poverty, school dropout, and repeat pregnancies—trapping them in cycles that perpetuate poor maternal health outcomes across generations.
High-Risk Regions in Africa (Sub-Saharan Africa Hotspots and Conflict Zones)

Sub-Saharan Africa remains the epicenter of high maternal mortality rates, especially in remote or conflict-affected areas. Countries like South Sudan, Chad, Nigeria, and the Central African Republic report some of the world’s worst maternal outcomes. In these hotspots, healthcare systems are often underfunded, understaffed, or completely inaccessible. Armed conflicts displace pregnant women and destroy essential health infrastructure, leaving them without prenatal care or safe delivery options.
Political instability also disrupts supply chains for medical equipment and drugs. Women are often forced to give birth at home or on the move, without skilled birth attendants—drastically increasing mortality risks.
The Effects of HIV/AIDS and Malaria on Maternal and Infant Outcomes
HIV/AIDS and malaria are dual health threats that worsen maternal mortality rates in Africa. HIV-positive pregnant women face higher risks of infections, anemia, and complications during delivery. If untreated, HIV can be transmitted to the baby during childbirth or breastfeeding. Meanwhile, malaria in pregnancy can lead to miscarriage, severe anemia, and low birth weight—factors closely linked to maternal and neonatal death.
Co-infections are especially dangerous, weakening the mother’s immune response and making it harder to recover from childbirth complications. Limited access to antiretroviral therapy (ART) and preventive malaria treatments further aggravates this deadly health burden across African nations.
Access to Skilled Birth Care and Emergency Obstetric Services

Access to skilled birth care and emergency obstetric services is vital in reducing maternal mortality rates across Africa. Skilled health professionals—such as trained midwives, nurses, and doctors—can identify complications early, provide life-saving interventions, and ensure safe deliveries. Yet, in many African regions, women deliver without any professional assistance due to a severe shortage of trained personnel and poorly equipped facilities.
Health centers may lack basic supplies like sterile gloves, blood transfusions, or even electricity. In some rural areas, there may be no health facility within reachable distance at all. Without immediate access to emergency obstetric care, conditions such as hemorrhage, obstructed labor, and eclampsia often prove fatal for both mothers and infants. This is why the Heart Hive Foundation is committed to supporting underserved communities with the critical resources they need to save lives.
Poor infrastructure and lack of transportation further compound the crisis. Many women live far from health centers and must travel long distances on foot, by bicycle, or via makeshift vehicles—often while in active labor. Unpaved roads, flooded paths, and unsafe terrain can delay critical care by hours or even days. In conflict zones or during rainy seasons, access becomes nearly impossible.
Ambulance services, if they exist, are often limited to urban areas or require out-of-pocket payments most families can’t afford. These “second delays”—the time it takes to reach care after the decision to seek help—are among the most deadly contributors to Africa’s high maternal mortality rates.
Innovative Programs and Heart Hive Making a Difference
Innovative programs and committed NGOs are proving that change is not only possible but already underway in the fight to reduce maternal mortality rates in Africa. Mobile clinics are reaching remote villages with life-saving care, mHealth tools are empowering women with timely information via their phones, and donor-funded initiatives are building maternity wards where none existed before. These efforts are bridging the gap between vulnerable mothers and the care they urgently need. By combining technology, grassroots involvement, and global partnerships, these solutions are turning despair into hope—one safe birth at a time. The path to ending preventable maternal deaths in Africa is long, but with innovation and collective will, it is absolutely within reach.
.png)



Comments